Small acts of kindness

On Thanksgiving Day of 2020, eight months into the COVID-19 outbreak in the United States, Susanne Walther, a palliative care nurse working in New Jersey, received a text message from the wife of a former patient who died in the early days of the pandemic. The wife said that she thought about Walther, 61, often and that she would never forget her.
The message was a reminder for Walther that “small acts of kindness stay with people forever.
”What had she done? She simply “didn’t let them throw away her husband’s belongings,” she recalled. “Even when people are acutely grieving the loss of someone they love, they still have the kindness in their hearts to reach out to the clinicians who have cared for them.”
As the director of the palliative care team at University Hospital, a 519-bed hospital in Newark, New Jersey, Walther works closely with patients close to death. This means that she often talks with families when her patients are near the end of their lives, which would sometimes wear on her mental health.
The year of the pandemic has taken a toll on health care staff. Many frontline workers have left their jobs because of the pressures. Those who continue this work, like Walther, report that they are sustained, in part, by the thanks and appreciation they get from patients and their families.
The message meant so much to Walther. It reminded her that while they could not always save those suffering from COVID, they could offer comfort to them and their families.
In the early days of the pandemic, nurses and other frontline workers were especially important because few visitors were allowed in hospitals. Family members dropped their loved ones at the door of the emergency room and might never see him or her again.
The wife who texted that she would never forget Walther was one of them. Her husband was sick at home last spring and did not come to the hospital until the last minute. The staff attempted resuscitation with CPR, breathing machines and life support, but he still died in less than an hour at the emergency room. Right before the staff took his body out of the emergency room, Walther noticed his bag of personal belongings underneath the stretcher, which would get thrown away soon.
During the pandemic family members often called the hospital about clothes, wallets or watches that belonged to deceased patients, but the items were already gone, Walther said.
“It was such a panic with COVID. People were so scared that sometimes the belongings would be thrown in the garbage,” Walther explained. “Nobody wanted to touch them. People thought if they opened up the bag, they would get infected.”
Walther did not want this to happen to the wife of this patient, so she took the man’s belongings and planned to return it to his wife.
A month later, the wife and Walther met outside of the hospital. She handed Walther the small tropical plant inside her husband’s bag of belongings and insisted on Walther keeping it.
She told Walther, “Your kindness was the only thing that pulled me through my husband’s death. I cannot thank you enough.”
Since then, Walther has been watering it once a week, and the plant is thriving in her office at the hospital.
Born in 1959, Walther graduated from Rutgers University in 1985 with a Bachelor of Science in Nursing and started working as a nurse in New Brunswick. To search for more challenging work, she quickly transitioned into the intensive care unit and worked as an ICU nurse for nearly 20 years.
From 1987 to 1990, Walther worked as an agency nurse in Bergen County, NJ. As an agency nurse, she got staffed in ICUs and critical care areas of different hospitals over the county based on needs. In 1990, Walther joined University Hospital.
Working night shifts from 7pm to 7am, she rotated all around different units in intensive care units, including the medical unit, the surgical unit, the trauma unit, and the neurological unit.
Patricia Murphy served as the director of the palliative care team at University Hospital until her retirement in 2013. She said that Walther is “one of the most specialties you will ever meet when it comes to caring for patients… families would tell me about this wonderful nurse who took such good care of the person they loved.”
After working in ICUs for 17 years, Walther burned out: “I found myself working very, very hard to keep people alive at all, you know, even though it appeared as if they were not going to survive.”
“I was just overwhelmingly morally distressed by some of the work that we were doing on people’s bodies. And I felt a great need to be sitting with families and talking to them instead of taking care of the patients,” Walther explained.
Around that time, Walther was thinking about graduate school programs, and Murphy suggested palliative care. In Murphy’s opinion, Walther already had all the skills needed to be an ICU nurse, but the skill she was missing was how to be with families in times of crisis.
In the following three years, Walther continued to work night shifts, split the duty of raising two children with her husband, and received her master’s degree in palliative care from New York University in 2005. Shortly after her graduation, Murphy hired Walther to join her team full-time at University Hospital as an advanced practice registered nurse.
“It was extremely morally and professionally satisfying to be moving into palliative care, and setting myself up to work with families, having meaningful conversations, and empowering them to have options and choices and making decisions about their loved ones,” Walther said.
Recently, Walther worked with a young woman in her late 20s, both of whose parents were critically ill after contracting COVID. Her father, only in his 50s, was on a ventilator at the hospital, while her mother was also on a ventilator at another hospital.
Having conversations with family members on the end-of-life of their loved ones can be tough, but Walther never shies away from those conversations. She felt obligated to inform the daughter that some families would find this type of prolonged life support unacceptable and wanted their loved ones to die peacefully, liberating them from the machines and the tubes.
Later that day, the mother of this young woman died at the other hospital. The daughter called the hospital and said that she wanted her father taken off life support and any treatments to be discontinued. As the medical note suggests, the daughter wished his father to have a natural death and be at peace with his wife who had just passed.
Walther still choked up when talking about this case. “I really didn’t want to call her and have this conversation because I knew it was going to be a very hard conversation,” Walther said. “And yet, I feel like if I never told her this and never gave her this opportunity, she never would have been empowered to consider that she could actually let her parents die on the same day and be together wherever she thinks they are, after they die.”
Although Walther has many intimate conversations with patients and their family members, she does not keep in touch with them afterward the service. However, working in a small community where many people have limited health care resources, Walther has helped multiple families through multiple losses.
After Murphy retired in 2013, Walther became the new director of the palliative care team at University Hospital. Currently, the palliative care team has four people, including two advanced practice registered nurses, one social worker, and one licensed counselor.
When COVID first hit New York City last year, tens of thousands of people died. The operating rooms at the hospital were closed, and most of the staff got relocated. Despite relocations, the palliative care team supports not only patients and families but also their colleagues at the hospital.
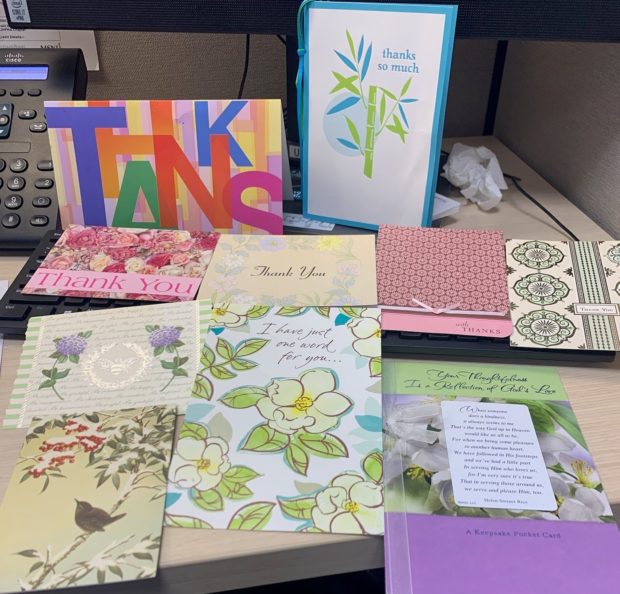
“One of the things our team was talking about, through the surge last year, was how little we felt that we could actually do for people,” Walther said. “But we have so many more thank you cards from families showing such appreciation for the smallest, tiniest way that we helped them connect with their loved ones.”
A family of nurses with mother and daughter in the same hospital
As published in Columbia Journalism
A family of nurses with mother and daughter in the same hospital
Gretchen Tarrant
The pandemic made them realize what they cherish the most.
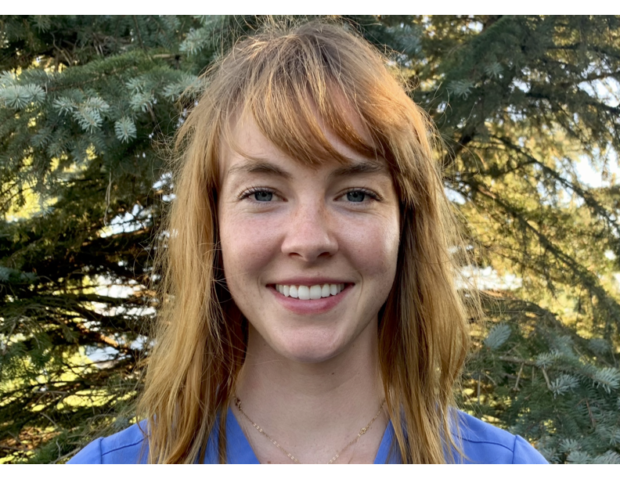
With her warm yet no-nonsense demeanor, Caitlin Hester almost seems like a born nurse, the kind you might expect to see on a season of Grey’s Anatomy; although her mother Darlene Hester, who pioneered as the nurse in the family, never anticipated seeing her daughter in scrubs.
Darlene Hester, 53, has worked as an intensive care nurse since 1991, and at the University of Vermont Medical Center in Burlington, Vt. since 1997, before her daughter was born. She later covered weekend shifts as she raised the younger Hester and her three siblings.
It is not uncommon for daughters to follow mothers into nursing. But what is unusual about the Hesters is that they work in the same hospital, in fact, in the same intensive care unit. In Darleen’s 30 years as a nurse, she has never met another mother-daughter combination working in tandem.
“My mom would always come home with interesting stories about her day,” Caitlin Hester, 25, recalled on her turn to nursing, “and I was interested in science, so it seemed like a natural fit.”
But that’s not quite how her mother remembers it.
“Caitlin came to shadow me once, and I was pretty busy, so I didn’t have a lot of time to talk,” Darlene Hester said,”but she didn’t ask me many questions, so I figured maybe it wasn’t for her.”
Call it fate, call it genetics, call it a high school student desperate for a summer job. Whatever the case, Caitlin Hester ultimately spent a summer as a nursing assistant at Starr Farm Nursing Center in Burlington, Vt. There, in between turning, cleaning, and administering medication, she met a patient that would change her life.
“He was an elderly man, dementia, high fall risk,” she said, rattling off his ailments like she was reading his chart. “But one day I started looking at the pictures above his bed. He was a World War II pilot. He had a beautiful wife, and kids. I could almost see his life unfolding in the pictures — in each one he got older. His kids grew up. I saw him riding bikes, doing things he liked. ”
It was a moment that Caitlin Hester continues to come back to on the hard days.
“He’s had a full life and done more things than I have. I think about that when I find myself getting numb,” she said.
But for those who know either Hester, “numb” is not the adjective of choice.
“Both Caitlin and Darlene have tremendous compassion for their patients. Both are great advocates,” Pat Delaney, an 18-year veteran at the University of Vermont Medical Center, said.
Delaney, 48, has worked with Darlene Hester for most of his career and was responsible for training Caitlin when she joined their ranks some years later.
After that summer at Starr Farm, Caitlin Hester went on to pursue a nursing degree at the University of Vermont while training as a cadet with the Reserve Officers Training Corps (ROTC). She graduated in May of 2018 with honors in both, landing a job in the critical care unit at Medstar Georgetown University Hospital in Washington, D.C.
“She’s definitely the most disciplined of the four of us,” said Joey Hester, Caitlin’s younger brother.
That discipline proved invaluable for her working on the surgical cardio-vascular floor at Medstar where there wasn’t room for error. One shift brought her to tears: it was an all-too-common scenario, she would learn; nurses juggling too many patients, families frustrated and angry, Hester and her colleagues caught in the middle.
“There’s not much emotional support for nurses sometimes,” she said. “Patients die. Then you’re on the list for a new patient.”
Caitlin Hester is now completing her certification as a registered nurse anesthetist at California State Fullerton/Kaiser Permanente.
 Of the eight nurses she started with, only one is left on the floor. The other seven have moved on to more relaxed roles, such as working in health care administration or going back to school. Caitlin Hester herself spent a year at Medstar before transferring back to the University of Vermont Medical Center in June 2019, where she wound up working on the same 25-bed surgical intensive care unit her mother has worked for 30 years.
Of the eight nurses she started with, only one is left on the floor. The other seven have moved on to more relaxed roles, such as working in health care administration or going back to school. Caitlin Hester herself spent a year at Medstar before transferring back to the University of Vermont Medical Center in June 2019, where she wound up working on the same 25-bed surgical intensive care unit her mother has worked for 30 years.
The transition wasn’t difficult. Despite Vermont’s lower pay and lagging staffing policies, it was a place that felt close to home with her mother around. But six months into her new job, COVID-19 reached US soil; a development that would bring her to tears more than once as she witnessed a multitude of lonely deaths.
By March 7, 2020, the state of Vermont registered its first presumptive COVID case, and her hospital’s management immediately separated critical care into COVID and non-COVID units to stave off potential spread of infections and deal with an anticipated surge in patients. Although the Hesters’ floor didn’t deal directly with COVID, their unit was far from untouched.
Shortly after the first confirmed case, all non-emergency surgeries were paused. As the state prepared for the onslaught of an unprecedented illness, the surgical ICU nurses (including both mother and daughter) were sent home.
Many of the nurses didn’t mind the time off at first, but as weeks stretched into months the lack of paychecks became worrisome.
And it wasn’t just the nurses that needed their paychecks; the hospital was going broke without its usual surgery premiums. Out of necessity for both the patients and the hospital, the surgical ICU resumed operations, but things were far from business as usual.
“During COVID a lot of us started to have really distressing death experiences,” Caitlin Hester said. “We weren’t even a covid floor, but they didn’t allow visitors. The worst deaths I’ve been a part of were ones where I was the only one in the room.”
Unfortunately, with COVID, suffering a lonely death was common. Throughout 2020, University of Vermont Medical vacillated between zero-tolerance visitation policies and thresholds of one or two people in cases where death was imminent. It’s a policy that doesn’t always sit well with the nurses on the floor.
Darlene Hester recalled a time when she admitted a father of three who suffered a severe head injury. He was dying, and at the time the hospital’s policy was to only allow two people to be with a person during the final moments. She asked herself, “which three kids should leave when their dad’s dying?”
The experience crystallized her conviction in advocating for her patients.
“When someone is scared and vulnerable and sick, it can be very frustrating for the staff, even when we’re aware this is bigger and beyond and just the here and now,” Delaney said.“We try as best we can, but when someone has a breathing tube in they can’t tell us; ‘I like NASCAR,’ or ‘Oh I like to knit.’”
Darlene Hester has done her best to advocate for a change in visitation policies, even writing letters to Governor Scott of Vermont — to no avail.
“This is a lifetime of agony you are providing for these families to live with the memory of never seeing their loved one,” Darlene Hester said.
Not only is the emotional toll heavy on families in end-of-life situations, but as both mother and daughter have experienced, the visitation policies also affect patient care decisions. Families who aren’t able to visit loved ones in the hospital often drag out the dying process in ways that may lead to a more painful death.
“When families can’t be in the hospital and they say: ‘do everything,’ often they can’t comprehend what ‘everything’ means without a visual,” Darlene Hester explained.
 Caitlin Hester offers an additional perspective. “Death can be a beautiful, loving thing. That’s why it’s really important to do it right.”
Caitlin Hester offers an additional perspective. “Death can be a beautiful, loving thing. That’s why it’s really important to do it right.”
Rather than burning out, Caitlin Hester has doubled down on nursing. She recently moved across the country to become certified as a registered nurse anesthetist (CRNA) at California State Fullerton/Kaiser Permanente. She also adopted a dog she named Doug, which, according to her family, really brings out the caretaker in her.
Darlene Hester has picked up more shifts at the hospital, working multiple 12-hour days a week now that her youngest child, Amy, has her driver’s license.
Her husband says she gets excited working back-to-back days at the hospital, since she knows she’ll be able to care for the same patients.
And, as Darleen Hester points out, there are always signs of hope that make it all worth it.
She recalls a sixteen-year-old girl a few years back who came in with what seemed like a terminal head injury. She had crashed while skiing on vacation with her family. The parents were, in her words, “a mess.” Somehow, their daughter not only survived, but regained her ability to walk, play music, and is now attending college. She returns to the unit every year for her necessary scans.
Darlene Hester smiled, “She’s our little miracle.”
Family Ties in Intensive Care Nursing
As published in Columbia Journalism
Family Ties in Intensive Care Nursing
Marissa Guiang

Dan Houchins had the day off from work, but quickly came to the hospital when his brother called. There was urgency in his voice. It was early March and the COVID-19 pandemic was just on the cusp of an explosion. As an intensive care unit nurse, Houchins, 28, was accustomed to high-pressure medical situations, but didn’t grasp the magnitude of what was to come.
“My brother called me from inside the hospital and said, ‘I need to meet with you, I have something for you,” Houchins said.
Unsure of what his brother needed to give him, Houchins rushed to meet him on the 7th floor of the hospital.
“You’re gonna need this,” his brother said, motioning to a large cardboard box on the floor. His brother then bent down, took out a big dual-pan respirator with two cans, and handed it over. Houchins inspected the device — it reminded him of the type of gas masks seen in war movies.
“Things are gonna get really bad in the next few months,” his brother said as he picked up the box, carrying an extra respirator to their sister who was working on another floor.
“When he handed me that mask, it really hit me. That was the moment I knew,” Houchins said. That same week, the University of Chicago Medical Center, one of the largest hospitals in Illinois with over 800 beds, transformed into a giant COVID-19 ICU. This was where Houchins and his siblings worked and battled the pandemic from the frontlines.
Houchins comes from a family of nurses. Not only are his brother and sister nurses, his parents also have nursing backgrounds. Now, Houchins’ father is the director of women and children’s health at Northwest Community Hospital, while his mother is the director of infection control at the Joint Commission, the nation’s largest standards and accreditation organization in health care. To round out an all-star family on the frontlines, Houchins’ younger brother is in nursing school at Loyola University Chicago.
Each member of the family was taking on the pandemic head-on on a daily basis. Alongside Houchins, they understood the pressures of being a nurse as hospital beds, personal protective equipment, and other medical resources became scarce. There was only one unit at Houchins’ hospital that was designated for non-COVID patients, and that was the cardiac ICU — his unit.
Starting in mid-March, every uninfected patient got reassigned to Houchins’ unit.
“All these different patients automatically came to us — neuro, bad bleeders, gunshot wounds, trauma. All these people my ICU unit doesn’t normally take,” he said.
Everyday, the cardiac ICU’s 32 beds were at capacity and the unit was bursting at its seams.
“Someone would die, we’d quickly clean up the room, and then in 15 minutes, a new person was in there,” he said.
Houchins remembered the period between May and October 2020 being the hardest his unit has ever had to work.
Houchins started his nursing career in the impatient cardiology unit at the University of Chicago Medical Center. But down the sterile, brightly fluorescent-lit hallway was the unit he yearned to work for: the cardiac ICU. With 32 beds and 120 nurses on staff, it’s the largest unit at the medical center and is known for its intensity.
After networking with other people in the cardiac ICU, going through multiple rounds of interviews, and ultimately proving himself with the work he did with his first unit, Houchins became a newly minted, 26-year-old ICU nurse in 2019.
The learning curve was steep, going from impatient care to ICU care. It took Houchins several months to learn the ropes from fellow nurses, but only so much training and technical repetition could prepare him for what his day-to-day work life would be for the next few years.
“You deal with a lot of death,” said Houchins. “I didn’t see much death prior to the ICU, and there’s no preparation for it in school. It’s just something you learn on the job.”
Houchins’ experience in the cardiac ICU ranges from peaceful monitoring of transitions, which is the unit’s word for death, to highly-stressful life-or-death situations. The latter is most common when the hospital has a code, the term for when a patient is in need of resuscitation efforts.
“A bunch of people come to the room and it gets pretty messy,” said Houchins. “And it can last for hours. You get ’em back and then they die again — it’s just on and off.”
After a code, he can sometimes be covered in sweat, blood, and other bodily fluids. “It can be crushing,” said Houchins. “But you have to accept that these things are part of your job.”
With a broad build and thick beard, Houchins gives off a tough presence. But like any other guy in his twenties, his Facebook photos show him having fun at parties and music festivals, surrounded by dozens of friends. He has a big smile and often makes silly faces at the camera.
Houchins grew up in Tinley Park, a south suburb of Chicago about 30 minutes from the city by car. After finishing high school, he moved to Peoria, Illinois to attend Bradley University, where a majority of his coursework was in business.
Houchins said his parents were supportive of him paving a different path for himself. But, in addition to being constantly exposed to his family’s experiences as nurses, Houchins credits his best friend and former roommate for his eventual interest in nursing. He eventually left Bradley University and enrolled at Chamberlain College of Nursing.
But just a few years after making that pivot, Houchins experienced a loss that shook him.
“My best friend, the one who got me onto this path to nursing, he died,” he said. The cause of death was an overdose of fentanyl, a synthetic opioid pain medication that can be up to a hundred-times more potent than morphine. Houchins’ friend was taking drugs from the hospital and used them for himself.
“After that happened, I had a really hard time giving my patients fentanyl at work,” said Houchins. “It just got to be too much, so I decided to go to therapy.”
Forming a barrier between work life and personal life can be very difficult at times. Houchins, as much as he tries to form that barrier, admits that it’s an ongoing challenge to keep the two separated, especially since statistically, someone dies in the cardiac ICU in his hospital every day, even in non-pandemic conditions.
“When I first started in the ICU, of course it was tough. But even now, nearly two years later, it’s still tough,” admits Houchins.
As much as working in the ICU is about saving lives, it’s also about letting life end in the best way possible. While saving lives is what Houchins strives to do in his career, he also says that being an ICU nurse is also about knowing when to let go of life.
“You go in there, you’re all gowned up, and you’re sweating your ass off the whole time, but you hold their hand and be there for them,” said Houchins. “You share that very moment together, right before death.”
The dying process in the ICU is standardized. The patient is usually hooked onto a morphine or fentanyl drip to reduce pain and increase sedation so that they aren’t gasping for air while they’re dying. Once the patient is no longer living, nurses pull out any old IVs, clean the body, and place the deceased in a body bag.
“I go through the motions once there’s no longer a pulse,” said Houchins. “But the dying process itself can take hours, even days. That’s when I really need to be there for the patient.”
And being there for the patient also means being there for the family.
“People deal with death differently, and oftentimes they don’t deal with it well, especially if they don’t understand what’s going on,” said Houchins. “Sometimes the best type of communication is allowing for silence, space, and processing. You have to know how to read the room.”
During the height of COVID in 2020, hospitals across the country had strict rules around visitors to protect patients, families, and hospital staff. At times, Houchins had to let his patients borrow his personal cell phone so that they could call their family members to say their goodbyes.
No one was an exception to those rules at the medical center. Last year, Houchins found himself in a situation where his own aunt was in the ICU, and his brother wouldn’t allow an exception for their own family.
“My brother’s decision was a testament that everyone has to do things they’re uncomfortable with in the ICU,” said Houchins. “Even when they don’t want to.”
While his aunt was not his officially assigned patient, Houchins assisted with her ICU care throughout her time in the hospital. He also served as her next of kin and was in charge of making end of life decisions on behalf of his aunt.
Despite his siblings working at the same hospital and his parents being within close geographic proximity, Houchins and his aunt’s son were the only relatives who were able to see his aunt before she died.
While the visitor rules in the hospital were not ideal due to the pandemic, Houchins and his family were still able to find some peace in an otherwise difficult situation. “I’m honestly kind of blessed that I had the privilege to take care of my aunt like that,” he said.
Through his experience in the ICU, Houchins has found a certain level of acceptance and comfort when it comes to “transitioning” a patient. To him, the decision to move from life-saving mode to comfort mode is when the care team has thoroughly exhausted all available options and resources.
“Dying doesn’t have to be this horrible, miserable thing,” said Houchins. “What’s worse is continuing to keep someone alive who shouldn’t be.”
At times, Houchins questions his decision to pursue such a career path.
“On a pretty regular basis, everyone in the ICU probably asks themselves, ‘Why the hell do we do this?’” said Houchins.
But every time he questions his career path, he remembers, “When I take a step back and see other people filling little juice cups, I’m reminded why I’m not doing that. I didn’t become a nurse to hand out juice.”
Houchins doesn’t intend to stay in the ICU for the rest of his career. His plan was always to do just five years in the ICU, two of which are already behind him. After he hits his 5-year mark, he aspires to either become a clinical support specialist or go back to school to become a certified registered nurse anesthetist.
While the work Houchins does is emotionally difficult as it is physically exhausting, what he’s gained from ICU nursing at the University of Chicago Medical Center is what he refers to as a type of fraternity — a brotherhood.
“We’re all suffering together in a weird way. It’s a tough job, but we’re really doing it together,” said Houchins. “It’s that unity that keeps a lot of us around.”
He says it’s hard for people outside of that circle to understand what ICU nurses go through on a regular basis.
“I often have friends who’ll text me, saying, ‘Hey how was work?’” Houchins said. He immediately has flashbacks of being covered in a patient’s blood or calling security on a patient’s family member after they’ve gotten violent towards staff, out of grief.
As someone who lives by himself, Houchins comes back to an empty apartment after a tough shift at work, day after day. But while he might be alone, he still has his family who knows what it’s like — just a text, phone call, or short drive away.
“They understand what I’m feeling and talking about, even if I don’t say much,” he said.
And that understanding is oftentimes all he needs.
DACA allowed her to work on the pandemic frontline, but her status is still uncertain.
As published in Columbia Journalism
DACA allowed her to work on the pandemic frontline, but her status is still uncertain.
Ella Creamer

Jessica Esparza, an intensive care unit nurse in a town in central Washington, was assigned her first coronavirus patient last spring. At the time, she felt like she had been punched in the stomach. She broke out into a sweat as she layered on her personal protective equipment.
She felt naked and vulnerable despite her PPE. Washington was the first state to confirm a positive test for the virus and it had only been a few weeks since its governor declared a state emergency due to exponentially increasing cases.
“We had no idea how this was going to go,” she said.
Her patient was scared too — they were short of breath and concerned for their family at home who may also have been infected. Esparza, 27, proceeded as well as she could, minimizing her exposure to the virus while maximizing care for her patient. She set a phone at the patient’s bedside and later stood behind the room’s window to call them for check-ups.
“It felt like the longest night in my life,” she said.
Esparza has been an ICU nurse at Central Washington Hospital in Wenatchee since December 2019. The small hospital has 198 beds and just over 1,300 medical staff.
She worked nights through the long pandemic stretch between March and September.
Like many of those working on the frontlines of the pandemic over the past year, Esparza came to the United States as a child and remains in the country legally under the Deferred Action for Childhood Arrivals program, commonly referred to by its acronym, DACA.
As a nurse, she has been the target of anti-immigrant comments. Yet, she takes care of every patient respectfully, “no matter what their views might be.”
Esparza hopes her work might remind Americans of the importance of welcoming immigrants into the US.
“We’re not bringing disaster or drugs or whatever you want to call it,” she said. “We want to improve our lives and improve the lives of the people around us.”
Esparza grew up in Durango, Mexico with her mother and younger sister. Just after she finished sixth grade, her mother moved the family to the United States to be with the family’s father, an agricultural worker who the family only saw once every two years.
The move was a shock for the 11-year-old: she had just selected a new school for seventh grade and was ready to start her classes.
“One random day we were hanging out with some friends and my mom came and picked us up and just said ‘We’re going to go to the United States to see your dad,’” Esparza said.
The children said a quick goodbye to their grandmothers, and soon after they were on a bus to the U.S.
When Esparza started school in her new Washington home, she knew very little English — only the letters and colors she had picked up in a Saturday English class that her mother had sent her to in Mexico. She became an easy target for bullies: they would pull her hair and close her locker in her face.
“They knew that I wouldn’t speak up and tell on them because one, I didn’t speak English, and two, I was shy,” she said.
After a fight broke out and two girls attacked her at school, the police became involved. Finally, the bullying stopped.
As a teenager, Esparza had ambitions of becoming a doctor. Nobody in her family had attended college — her parents didn’t make it to high school. But she was determined to go further and to pursue work that helped others. “When I was in school, I was the one in charge of the medical kit,” she said. “If someone cut their knee, here I was with alcohol and cotton swabs.”
Her undocumented status soon became a stumbling block, however, since she was ineligible for federal financial aid for college. Even though she was accepted to the University of Washington — one of the top universities in the country and her dream school — she lacked the funds to go.
So, she turned to nursing as a more viable way forward. She ended up studying for an associate’s degree at a community college to get prerequisites for nursing and did “everything possible” to pay for it, including working in blueberry and raspberry fields during the summer.
In 2012, the Obama administration brought in DACA, an immigration policy that allowed undocumented children to get a work permit in the US. This opened up a path for Esparza to pursue nursing school, from which she graduated in 2015. “It felt like all of the puzzle pieces were falling into place,” she said.
But her immigration status came with a great deal of uncertainty. Former President Donald Trump launched assaults on migrant communities almost as soon as he took office in 2017, with actions ranging from the Muslim Ban — an immigration restriction targeted largely at Muslim-majority countries — to his branding of most Mexican immigrants as “bad hombres.” He also attempted to phase out DACA.
“I felt like I was hanging by a thread,” she said of the Trump years. If the program went away, her job would probably have to let her go.
Trump’s attempt to phase out the program, however, was met with a slew of lawsuits. At the height of the coronavirus spread last summer, DACA reached the Supreme Court. In a 5–4 decision, the court ruled that the proposed phase-out would be “arbitrary and capricious.”
“There was a pandemic going on, and the thing that I was worried about was that I was going to lose my work permit and not be able to take care of people that needed my skills,” she said.
Ultimately, Esparza ended up caring for many coronavirus patients, and through her work during the pandemic she became intimately familiar with the final moments of patients’ lives.
Dealing with death has been an inevitable part of her job over the past year. The pandemic restrictions added a new dimension to end-of-life care in the ICU: just two people were to be permitted to visit a dying patient. Often, no family members are present when a patient passes away — relatives might be scared of coming to the hospital or may no longer have the means to travel after being financially impacted by the pandemic.
Here, Esparza takes on the role of a social worker. She must bridge the patient-family gap. This sometimes takes the form of organizing a virtual goodbye via Zoom. Typically, the nurse will establish a good time for a call with the immediate family, who will pass the message on to the patient’s loved ones.
“We have two iPads in our unit that we can wheel around,” she said. Often, the patient cannot communicate with the family — perhaps they are sedated, or silenced by invasive equipment. “You just set this iPad in front of them so that the family can see their loved one.”
Esparza always tried to make patients look as good as possible for the calls. On one occasion, she braided a patient’s hair. Each time a family member joined the meeting, they would comment: “Oh my gosh, their hair is so pretty, who did that?”
Bearing witness to so much death has been hard for the nurse, and she recently sought therapy.
“She did struggle with the amount of loss that we had in our unit,” one of her supervisors and ICU charge nurses Janet Wilde said. Yet, Esparza maintained both a deep compassion for patients and sense of humor throughout, Wilde, 63, added.
Esparza talks through distressing emotions with her coworkers and husband, a food scientist who is currently taking a break from work. They hike, play video games together, and last year got married in a small ceremony.
“He’s white, and he’s been super open to hearing my struggles. He enjoys being part of my culture, learning the language, and being a part — as much as he can — of my family and our traditions,” she said.
Indeed, family is everything to Esparza. Having worked her way through higher education, she is a trailblazer for her three younger siblings.
“She’s the first in our family to take on a lot of the struggles that come with being a student here in the United States,” her younger sister Silvia Esparza said. “Everything that she did has helped me through my path.”
The desire to help others is a common thread between the sisters, with the younger studying to be an educator. “That runs in our family and within our blood, just to be servants to the communities we are part of,” Silvia said.
Beyond her set responsibilities as a nurse, Jessica Esparza has become a representative of her local DACA peer group. While she used to fear telling coworkers about her background, she now openly speaks about her status in the hope that it will change perceptions of immigrants in some small way.
“If I wasn’t advocating for myself, then who was?” She said she feels a responsibility to speak on behalf of those who are undocumented. “I felt like I had this power and I needed to put it to use.”
Esparza plans to stay working in the ICU: she enjoys the focused care of one to two patients at a time. Now, her real ambition is to feel secure in the US.
“My hopes and dreams are that one day I can be certain of my status in this country and feel like I belong here, since I’ve been here more time than I’ve been in Mexico,” she said. “I can’t wait for that day.”
Trials of an ICU nurse during a pandemic
As published in Columbia Journalism
Trials of an ICU nurse during a pandemic
Nidhi Upadhyaya

Nothing in her 15 years as an Intensive Care Unit nurse prepared April Weirich for the hardships and challenges of COVID-19.
When the pandemic hit in March last year, she was working in the 32-bed ICU of Lancaster General Hospital in Lancaster, PA.
“I can remember when it first started,” Weirich recalled. “We didn’t know anything — what we were dealing with or how contagious it was.”
Weirich, 38, made it through the first wave of the pandemic in the ICU, and after she graduated from Millersville University with a qualification as a nurse practitioner in September of 2020, she was promoted to Hospitalist in Internal Medicine. While she had made a decision to move on from her role as an ICU nurse, the pandemic reinforced it. Her new position, which is similar to that of a physician, has her seeing several patients for brief periods of time, unlike spending 12 hours with the same patient as an ICU nurse.
Weirich spoke about her life and career in a Zoom interview from her home, just a year after the start of the pandemic. She wore a deep blue hoodie and her light brown hair was up in a bun. Her green eyes had a faraway look in them as she spoke.
Weirich said that she wanted to work as a health professional since she was in high school. For a brief period, Weirich contemplated studying genetics but it was only when her mother said that she needed to be around people and not be stuck in a lab that she gave up the thought.
Born and raised in Lancaster, Weirich got her bachelor’s degree in nursing 100 miles away at the Bloomsburg University of Pennsylvania. It was during this time that her father Craig was diagnosed with stage four colon cancer.
They knew he wasn’t going to make it. Her decision to become a nurse was reaffirmed when she saw how well the nurses treated her father during his treatment. “I wanted to help people and sometimes helping people is guiding them through the end days of their lives,” she said.
When it came time to pick a unit to work after college, Weirich chose the ICU. Weirich still remembers her early days as a nurse. She was 22 and fresh out of college.
“It was terrifying,” she said. “I saw how sick people can be and that I can’t always make people better.”
She started with night shifts, and it took her a while to adjust to the schedule. The lack of sleep worsened her anxiety as she took care of patients in the hospital. Her most vivid memory is from the day she had a patient who coded — or, in technical terms, underwent cardiac arrest — and ended up dying. She was fine when it happened, but as soon as she reached home, she was hysterical.
“I was so young and so afraid of doing something wrong,” she said. “The more you deal with it, the more you get used to the fact that these things happen and we’re not in control of everything as much as we wish we were.”
Over the years, Weirich found it helpful to keep some emotional distance from her patients. This coping mechanism helped her process her emotions after a long day at work.
 Her older brother Craig, named after his father, once asked her, “What exactly do you do?” She replied, “I am whoever my patients need me to be. I go into one room and I’m a cheerleader. I go into the next and I have to be someone’s mom. And in the next, someone is dying so I’m compassionate.”
Her older brother Craig, named after his father, once asked her, “What exactly do you do?” She replied, “I am whoever my patients need me to be. I go into one room and I’m a cheerleader. I go into the next and I have to be someone’s mom. And in the next, someone is dying so I’m compassionate.”
Ten years into her nursing career, another tragedy struck her family in 2016. Her brother Craig died of a heart attack at the age of 37. It took her back to the early days when she felt like she couldn’t make a difference. His death made it particularly hard for her to go back to work.
Her relationship with dying patients has always been complex. Some of her hardest patients were those that were living their last moments and the laws demanded that the team keep working on them. It was extremely hard to keep fighting battles they knew they were going to lose all along.
On the other hand, some of her most meaningful moments were with patients who knew they were going to die. “If I’m able to ease some of that transition, even if it’s morphine or just emotional support, it means a lot,” she said.
During the height of the pandemic, Weirich’s six months in the ICU took a toll. In the beginning of 2020, the hospital nurses would try to keep nurses with health conditions or pregnancies out of the ICU dedicated for Covid-19 patients. But as the case numbers spiked, nobody had a choice anymore. Older nurses in the hospital had started getting their wills in order, younger nurses with kids were looking for alternative living arrangements and a few others were just hoping to make it through the day safe and sound.
On top of their normal duties, nurses were asked to clean rooms, struggle into isolation suits, and spend time on phone and video calls with families of patients. The hospital offered meditation breaks for only 15 minutes of reprieve. She scoffed, “Most of us weren’t getting lunch breaks. If we got 15 minutes, we were shoving a sandwich down our throats.”
Prior to the pandemic, the staff supplied their own scrubs. But as Covid-19 hit, they were worried about carrying the potentially infected clothes back home and had demanded the hospital supply them with an extra set to wear during work hours.
“We had to fight for the scrubs, but they eventually provided them,” Jessie Stefanescu, another ICU nurse, said. “We had goggles but they fit terribly. They would fall off. So, a majority of the nurses brought their own.”
They were told that N95 masks could be cleaned and surgical masks could be worn for a week. Stefanescu said, “They said there is a nationwide shortage. Two years ago, if you had a patient, you literally had a new mask every time you went into the room. Now we were using them for weeks on end.”
The normal of everything had changed. There wasn’t much time to question things or just fight back against it because they were all just trying to put their heads down and try to do what was necessary.
While other nurses were navigating personal relations during the pandemic, Weirich was grateful that she lived alone and didn’t have any kids. She didn’t have to worry about infecting anyone.
Towards the end, once she left the ICU, she realized how bad the environment was for their mental health. Nurses who were in the ICU towards the end of the year — when only the sickest patients were admitted there — saw death daily.
When she moved to her new job as a Hospitalist, she felt a sense of relief. She was very close to a burnout and was glad she had an out.
“It was hard seeing her as stressed as she was and not being able to be there,” her mother said.
Now, she can be found in the hospital in her favorite royal blue, wide-leg scrub pants and long sleeve t-shirts, doing her daily rounds and conducting meetings with nurses.
When Weirich moved into her new house recently — a project she took on during the pandemic along with her master’s degree — five of her nurse friends were there with their husbands to help.
A lot of friends she had that didn’t work in healthcare kind of fell by the wayside during the years, she said. The more she worked as a nurse, the less she had in common with them.
“Your filter gets a little funny and people don’t get it,” she said.
Now that she works one week on and one week off, Weirich hopes that she can think about romantic relationships again. Having gone into nursing at a very early age, she couldn’t dedicate the time to meeting and getting to know new people.
“By the time I came home from work, I was peopled out,” she said. “I would have to sit and decompress for an hour before I could even function to make dinner. So how can I try and start a relationship when I need so much to take care of myself?”
With her new free time, she is looking forward to traveling, working out and gardening again once Spring arrives and the weather is more pleasant. Her new house features a pool and a yard that her adopted dogs Fiona and Penny love to play in.
The pool is also new to her. Having never had one before, she went to the store to discuss what was needed to maintain it. The employee asked her if she would be able to handle it.
“How hard can it be? Cleaning a pool is basically dialysis,” she said.





